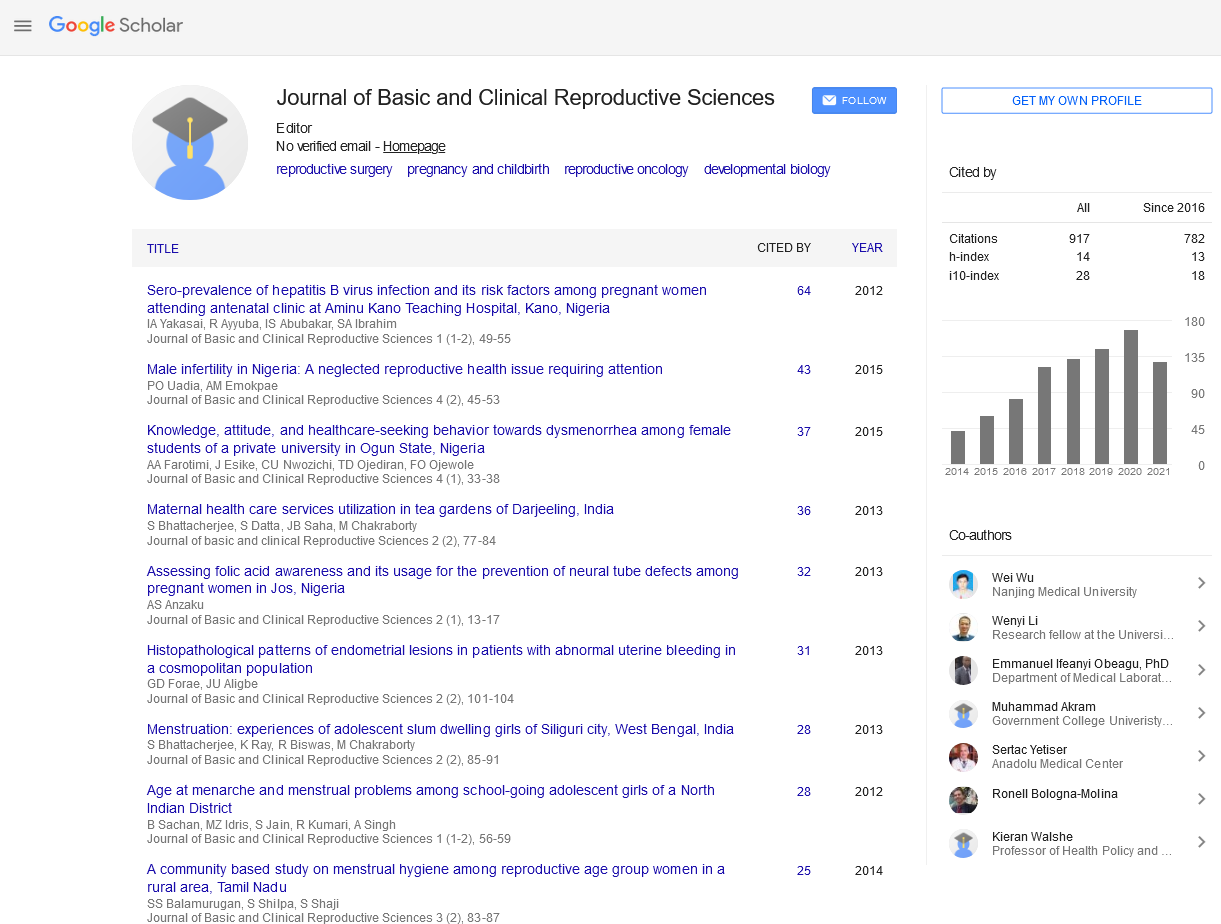
Original Article - Journal of Basic and Clinical Reproductive Sciences (2017) Volume 6, Issue 2
Knowledge and Perception of Pregnant Women to Episiotomy in Ibadan
Received: 25-Sep-2017 Accepted Date: Dec 02, 2017 ; Published: 12-Dec-2017
Citation: Oluwasola TAO ,Folasade A.Knowledge and Perception of Pregnant Women to Episiotomy in Ibadan doi: 10.4103/2278-960X.194508
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Episiotomy is the most common obstetric procedure for prevention of perineal laceration during childbirth. In order to further involve women in the decision-making process for their care, understanding their perception of common obstetric procedures will contribute to practical discussions on the gaps that need to be filled.
Methods: Cross-sectional descriptive survey of consenting pregnant women attending antenatal clinic at the University College Hospital, Ibadan. Information on their socio-demographic data, knowledge and perception about episiotomy was obtained using an interviewer-administered questionnaire. Data analysis was done with SPSS version 18.0.
Results: A total of 304 women were interviewed, of which 199 (65.5%) had ever heard about episiotomy. Among those ever heard, 62 (31.2%) have had personal experience with 10 (16.1%) reporting sexual dysfunction as complication. Only 60 (19.7%) are ever willing to accept episiotomy while 172 (56.6%) will advise friends and relatives against acceptance. Only parity is significantly associated with knowledge (X2 – 15.08, p<0.001) while age is associated with previous experience (X2 – 22.92, p<0.001). Previous experience had no effect on willingness to accept repeat episiotomy (OR = 1.24; 95% CI: 0.63 – 2.44). Health workers are the main source of information.
Conclusion: Parturients in our environment are yet to accept episiotomy due to inadequate information as many of them believed it is unnecessary. Sessions on intrapartum interventions in obstetrics need to be further integrated into our antenatal care services.
Keywords
Childbirth, Episiotomy, Perineal laceration, Sexual dysfunction.
Introduction
Episiotomy, the surgical incision made to widen the perineum in order to facilitate vaginal delivery and prevent laceration, has been part of obstetrics practice since 1920s [1,2] although said to have been reported as far back as 1741 [3]. Primigravidity and operative vaginal deliveries have been associated with higher incidence of episiotomy and while routine use with its attendant complications have continued unabated, restrictive use recommended by WHO has been difficult to achieve in many developing countries [4,5]. Randomized controlled trials comparing routine with restrictive use of episiotomy during spontaneous vaginal birth suggested that adopting a restrictive policy offers significant benefits to the parturient especially a reduction in the risk of posterior perineal tears [6].
It has been shown that women were offered little or no information by healthcare professionals on the essence of episiotomy while the parturients’ level of awareness of episiotomy has not been well documented in our environment as earlier emphasis were focused on indications and complications [7]. Documented complications of episiotomy include post-episiotomy discomfort, infection and sexual dysfunction [2,8-11]. However, the goal of informed choice ensures that pregnant women are provided with comprehensive information about their care in order to facilitate appropriate and informed decisions [12-16].
A greater understanding of implication of episiotomy from the perspective of the women will assist in improving the quality of care in the postpartum period for those who underwent the procedure. This study was therefore aimed to provide information on what women know and perceive about episiotomy and determine the possible factors that influence their attitude towards it.
Methodology
This is a descriptive cross-sectional survey conducted among pregnant women within Ibadan metropolis over an 8-week period. Consenting pregnant women in the antenatal clinics of the University College Hospital, Ibadan – a tertiary level health care centre, and Adeoyo Maternity Hospital, Yemetu, Ibadan (providing secondary level care) were enrolled into the study. Ethics approval was obtained from the Oyo state ethics committee. Data were collected using structured interviewer-administered questionnaire with both open and closed ended questions. Information obtained using set questions on the questionnaire included: the respondents’ sociodemographic characteristics (by asking questions on age, marital status, level of education, tribe and occupation); knowledge about episiotomy and the source(s) of information; personal experiences of episiotomy including indication, the accoucheurs as well as complications if any; acceptability of episiotomy to the respondents as well as opinion about health workers’ attitude towards performing episiotomy.
The data were coded, cleaned and checked for completeness. Frequencies, proportions and percentages were generated for socio-demographic variables and variables under the knowledge and attitudes of pregnant women to episiotomy. Chi square tests were used to determine associations and odds ratio with confidence intervals were calculated for risks while p-value less than 0.05 was set as statistically significant. Statistical analysis was done using SPSS version 18.0 (Chicago, IL, USA).
Results
Three hundred and four (304) pregnant women, with mean age 29.6±4.8 years, satisfactorily responded to the survey, out of which 199 (65.5%) had ever heard about episiotomy. The socio-demographic details were as presented in [Table 1].
| Variable | Frequency | Percentage |
|---|---|---|
| AGE (years) | ||
| 16 – 20 | 7 | 2.3 |
| 21 – 25 | 53 | 17.4 |
| 26 – 30 | 133 | 43.8 |
| 31 – 35 | 75 | 24.7 |
| 36 – 40 | 33 | 10.9 |
| > 40 | 3 | 1.0 |
| TRIBE | ||
| Yoruba | 278 | 91.4 |
| Igbo | 11 | 3.6 |
| Hausa | 5 | 1.6 |
| Others | 10 | 3.3 |
| RELIGION | ||
| Christianity | 169 | 55.6 |
| Islam | 135 | 44.4 |
| MARITAL STATUS | ||
| Single | 3 | 1.0 |
| Married | 301 | 99.0 |
| PARITY | ||
| Nulliparous | 123 | 40.5 |
| Primiparous | 76 | 25.0 |
| Multiparous | 102 | 33.5 |
| Grandmultiparous | 3 | 1.0 |
| LEVEL OF EDUCATION | ||
| Primary | 24 | 7.9 |
| Secondary | 108 | 35.5 |
| Tertiary | 172 | 56.6 |
| OCCUPATION | ||
| Professional | 65 | 21.4 |
| Artisan | 57 | 18.8 |
| Trader | 124 | 40.8 |
| Civil Servant | 22 | 7.2 |
| Unemployed | 36 | 11.8 |
| EVER HEARD ABOUT EPISIOTOMY | ||
| Yes | 199 | 65.5 |
| No | 105 | 34.5 |
Table 1: Socio-demographic characteristics of the respondents.
Majority, 181 (59.5%), of the respondents were multiparous, 278 (91.4%) were of the Yoruba tribe and about 81.6% of those who had ever heard about episiotomy had good knowledge although only about one-third, 34.2%, got their information about episiotomy from the healthcare providers [Table 2].
| Variable | Frequency | Percentage |
|---|---|---|
| Health workers | 104 | 52.3 |
| Peers / Friends / Neighbours | 57 | 28.6 |
| Family | 12 | 6 |
| Media/Books/Internet | 8 | 4 |
| Antenatal Clinic | 7 | 3.5 |
| Missions/Maternity Homes | 6 | 3 |
| Others | 5 | 2.6 |
Table 2: Sources of information on Episiotomy.
All women who had ever given birth, 62 (34.3%) have had episiotomy representing about one-third, 31.2%, of women who have heard about episiotomy and 20.4% of the study population [Table 3]. Ten (16.1%) of those who have had episiotomy previously performed on them claimed to have had sexual dysfunction in form of dyspareunia, lax vaginal wall and loss of libido as complications. Fetal macrosomia remained the commonest indication for episiotomy and out of the respondents who have had episiotomy previously, 38 (61.3%), were informed before the procedure and provided verbal consent. Majority, 140 (70.4%), of those who have heard about episiotomy disagreed with its routine use with 70 (35.2%) suggesting extensive preparation of pregnant women for the procedure antenatally while 61 (30.7%) stated that episiotomy could be a risk factor for HIV infection. In general, about onefifth, 60 (19.7%), of our respondents will be willing to have an elective episiotomy if indicated while 172 (56.6%) stated that they will discourage their friends and relatives from accepting an elective episiotomy.
| Variable | Frequency | Percentage | |
|---|---|---|---|
| Ever had episiotomy | |||
| Yes | 62 | 34.3 | |
| No | 119 | 65.7 | |
| Acceptability of Episiotomy when indicated | |||
| Acceptable | 60 | 19.7 | |
| Not acceptable | 224 | 73.7 | |
| Not sure | 20 | 6.6 | |
Table 3: Experience and Acceptability of Episiotomy.
Parity has a statistically significant association with knowledge of episiotomy (X2=15.08, p<0.001) unlike age, educational status and occupation. Age is however significantly associated with experience of episiotomy (X2=22.92, p<0.001; table 4). Acceptability of episiotomy is unaffected by past experience (OR = 1.24; 95% CI: 0.63 – 2.44; P = 0.529) as only 22.6% of those with previous episiotomy are willing to have a repeat [Table 4]. There were no statistically significant differences in the acceptance of an episiotomy with respect to parity (X2 = 0.112, p = 0.946), tribe (X2 = 0.018, p = 0.999), level of education (X2 = 0.026, p = 0.987), occupation (X2 = 2.954, p = 0.566) and religion (X2 = 0.528, p = 0.467). In addition, respondents with previous experience are likely to accuse the health workers of using episiotomy unjustifiably only when they have complications such as sexual dysfunction (OR=2.56, CI = 1.64 – 3.48). Their advice to friends and relations who may need episiotomy is unaffected by their personal experiences (OR= 0.84, P = 0.702).
| Awareness of episiotomy | |||||||
|---|---|---|---|---|---|---|---|
| Parity | Yes, N (%) | No, N (%) | Chi square | P – value | |||
| Nulliparous | 66 (53.7) | 57 (46.3) | 15.082 | < 0.001 | |||
| Primiparous | 51 (67.1) | 25 (32.9) | |||||
| Multiparous | 82 (78.1) | 23 (21.9) | |||||
| Have you had an episiotomy performed on you? | |||||||
| Age groups (years) | Yes N (%) | No N (%) | Chi square | P – value | |||
| ≤ 25 | 4 (11.8) | 30 (88.2) | 22.919 | <0.001 | |||
| 26 – 30 | 22 (26.2) | 62 (73.8) | |||||
| 31 – 35 | 18 (33.3) | 36 (66.7) | |||||
| > 35 | 18 (66.7) | 9 (33.3) | |||||
| Have you had an episiotomy performed on you? | |||||||
| Parity | Yes N (%) | No N (%) | z - statistic | p-value | |||
| Primiparous | 20 (26.3) | 56 (73.7) | |||||
| 1.648 | |||||||
| Multiparous | 42 (40.0) | 63 (60.0) | 0.099 | ||||
| OR = 0.589; 95% Confidence Interval: 0.314 - 1.105 | |||||||
| If you require an episiotomy, would it be acceptable to you? | |||||||
| Previous experience | Yes N (%) | No N (%) | z – statistic | p – value | |||
| Ever had an episiotomy | 14 (22.6) | 48 (77.4) | |||||
| Never had an episiotomy | 46 (19) | 196 (81) | 0.63 | 0.529 | |||
| OR = 1.24; 95% Confidence Interval: 0.632 – 2.444 |
Table 4: Factors associated with Episiotomy.
Discussion
The involvement of parturients in decision making process for their care, as well as provision of up-to-date information about every obstetric procedure they may require in facilitating safe delivery, has great potential in ensuring optimal birth preparedness and complications readiness. We evaluated 304 parturients and found out that a significant number of the respondents have negative perception of episiotomy. Although about onethird of respondents who have heard about episiotomy have had personal experiences, more than half of them were willing to discourage their friends from accepting the procedure when needed.
The knowledge of episiotomy found among parturients in Ibadan is similar to a report from Calabar in 2012 but lower than a similar report from Kano in 2015 suggesting a possible status quo in efforts aimed at increasing awareness among pregnant women [12,14]. The major source of information was however the health workers – a clear deviation from previous reports which found families and friends as commonest sources of information [12]. In addition, the prevalence of episiotomy in this study is higher than 27.3% reported by Adekanle et al. about a decade earlier [17] although similar to the rate reported by Alayande et al. in 2011[4] implying a fairly constant rate for the study environment despite the 10% recommendation by the WHO for normal deliveries [17-19]. In contrast to Abubakar and Inyang-Etoh’s reports, [12,14] more than three-fifths of our respondents were informed about episiotomy before the procedure. This is an improvement that should be sustained as it is expected that all patients should provide a written or verbal informed consent before any clinical or surgical procedure.
Sexual dysfunction has been associated with episiotomy in previous reports [5,20] and about one-sixth of the respondents who have had previous experience of episiotomy reported such, a slightly lower value than 22.5% previously reported by Bello et al from the same environment [5]. The attitude to episiotomy is strongly associated with previous experience as respondents who had never experienced an episiotomy were more likely to refuse one if required probably because of apprehension associated with labour and the belief that childbirth should be without any form of intervention [13]. In addition, presence of a complication is blamed on the health workers’ injudicious use of episiotomy – a reason to warrant provision of adequate information antenatally about these procedures and their possible complications. Appropriate counseling in the labour ward and obtaining consent before the procedure will further reduce the negative perception of the role of healthcare providers in performing episiotomy.
In the review of episiotomy for vaginal birth by the Cochrane Collaboration, it was concluded that a restrictive policy in the use of episiotomy should be recommended for practice [16]. This followed a significant reduction in the risk of clinically relevant morbidities such as severe perineal trauma especially posterior perineal trauma and healing complications in seven days found among the group that applied a restrictive use to episiotomy. There is an additional advantage that restrictive episiotomy has the potential to lower the risk of postpartum female sexual dysfunction [20]. However, for operative vaginal deliveries, a routine approach to use of episiotomy did not appear to significantly affect the risk of anal sphincter tears compared with restrictive use [21]. Applying the outcome of this review to regular practice may positively influence the perception of the patients to episiotomy. The restrictive episiotomy policy has also been adjudged to be cost effective when compared with routine policy [22]. Further research will be important in this area in view of the corresponding neonatal benefit and with respect to the study environment as episiotomy has been associated with lower first-minute Apgar scores among primigravida when compared with those who did not receive an episiotomy [23].
Parturients in the study environment are yet to be adequately informed about episiotomy. Health workers who perform the procedure are believed to be taking undue advantage of their ignorance and perform routine episiotomy thus increasing the incident rates in our environment. There is a need for adequate enlightenment of parturients on this surgical procedure through appropriate health talks on episiotomy using audio-visual aids such as videos during antenatal visits to increase awareness and influence a favourable positive attitude. In addition, the need for training and re-training of health care providers on current best practices for improving maternal and child health cannot be over-emphasized while integration of sessions on intrapartum obstetrics interventions into our antenatal care services will contribute positively to birth preparedness and complication readiness.
REFERENCES
- Beech BL. The History of Episiotomy in the United Kingdom. Assoc Improv Matern Serv. 2004;1–4.
- Perera YAG, Fernando TRN. Comparison of episiotomy rates, practice of analgesia and the maternal complications within first 24 hours at two tertiary care units : a comparative, descriptive and a retrospective study. Sri Lanka J Obstet Gynaecol. 2013;35: 10–5.
- Otoide VO, Ogbonmwan SM, Okonofua FE. Episiotomy in Nigeria. Int J Gynecol Obstet. 2000;68: 13–7.
- Alayande BT, Amole OI, OlaOlorun DA. Relative frequency and predictors of episiotomy in Ogbomoso, Nigeria. Internet J Med Updat. 2012;7:41–4.
- Bello FA, Olayemi O, Aimakhu CO, Adekunle AO. Effect of Pregnancy and Childbirth on Sexuality of Women in Ibadan , Nigeria. ISRN Obstet Gynecol. 2011;2011(Article ID 856586):6 pages.
- Carroli G, Mignini L. Episiotomy for vaginal birth (Review). Cochrane Database Syst Rev. 2012;(Issue 1):CD000081. DOI: 10.1002/14651858.CD000081.pub2.
- Owa OO, Eniowo AR, Ilesanmi OS. Factors associated with episiotomy among parturients delivering in a tertiary care centre in Nigeria. Int J Res Med Sci. 2015;3:836–40.
- Chigbu B, Onwere S, Aluka C, Kamanu C, Adibe E. Factors influencing the use of episiotomy during vaginal delivery in South Eastern Nigeria. East Afr Med J. 2008;85:240–3
- Scott JR. Episiotomy and Vaginal Trauma. Obstet Gynecol Clin North Am. 2005;32:307–21.
- Ho JJ, Pattanittum P, Japaraj RP, Turner T, Swadnpanich U, Crowther CA. Influence of training in the use and generation of evidence on episiotomy practice and perineal trauma. Int J Gynecol Obstet. 2010;111:13–8.
- Leal I, Lourenço S, Oliveira R, Carvalheira A, Maroco J. Sexual function in women after delivery : Does episiotomy matter? Health. 2014;6:356–63
- Abubakar MY, Suleiman MM. Perception of episiotomy among pregnant women in Kano, North ‑ Western Nigeria. Niger J Basic Clin Sci. 2015;12:25–9.
- Berg A, Yuval D, Ivancovsky M, Zalcberg S, Dubani A, Benbassat J. Patient perception of involvement in medical care during labor and delivery. IMAJ. 2001;3:352–6.
- Inyang-Etoh EC, Umoiyoho AJ. The practice of episiotomy in a university teaching hospital in Nigeria : How satisfactory ? Int J Med Biomed Res. 2012;1:68–72.
- Oyo-Ita AE, Etuk SJ, Ikpeme BM, Ameh SS, Nsan EN. Patients’ Perception of Obstetrics Practice in Calabar, Nigeria. Niger J Clin Pract. 2007;10:224–8.
- Society of Obstetricians and Gynaecologists of Canada, Association of Women’s Health Obstetric and Neonatal Nurses of Canada, Canadian Association of Midwives, The College of Family Physicians on Canada. Joint Policy Statement on Normal Childbirth. J Obstet Gynaecol Canada. 2008;30:1163–5.
- Adekanle DA, Olayemi OO. Episiotomy Rate and its Predictors among the Parturients at University College Hospital, Ibadan. Niger Med Pract. 2006;50:78–80.
- Garba I, Ozegya MS, Abubakar IS, Ayyuba R. Episiotomy at Aminu Kano Teaching Hospital, Kano, Nigeria: A 3-Year Review. Arch Int Surg. 2016;6:17-21.
- Baker PN. Operative intervention in Obstetrics. In: Baker PN and Kenny LC, Eds. Obstetrics by Ten teachers.19th ed. Published by Bookpower. 2011. Pp 224 – 240.
- Sayasneh A, Pandeva I. Postpartum Sexual Dysfunction : A literature review of risk factors and role of mode of delivery. Br J Med Pract. 2010;3:1–5.
- Murphy DJ, Macleod M, Bahl R, Goyder K, Howarth L, Strachan B. A randomised controlled trial of routine versus restrictive use of episiotomy at operative vaginal delivery: A multicentre pilot study. BJOG. 2008;115:1695–702.
- Borghi J, Fox-Rushby J, Bergel E, Abalos E, Hutton G, Carroli G. The cost-effectiveness of routine versus restrictive episiotomy in Argentina. Am J Obstet Gynecol. 2002;186:221–8.
- Izuka E, Dim C, Chigbu C, Obiora-Izuka C. Prevalence and predictors of episiotomy among women at first birth in Enugu , South ‑ East Nigeria. Ann Med Health Sci Res. 2014;4:928–32